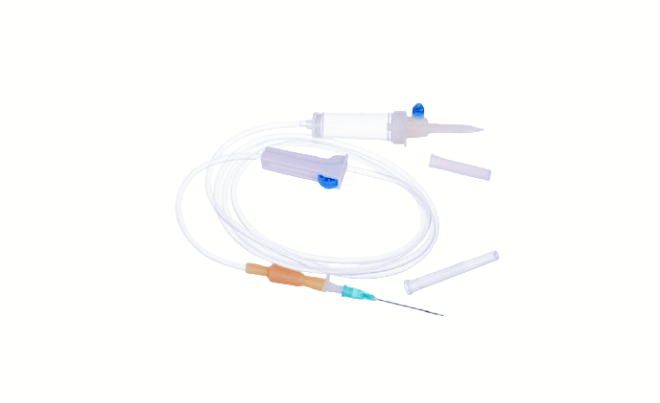
Proper administration of IV sets is essential for ensuring patient safety and treatment effectiveness. Let’s explore some best practices and guidelines for IV set administration:
- Selecting the Right Set: Choose the appropriate IV set and components based on the patient’s needs, treatment plan, and medical condition. Consider factors such as infusion rate, compatibility with medications, and patient comfort.
- Aseptic Technique: Follow strict aseptic technique during IV insertion and administration to minimize the risk of infection. Use sterile gloves, clean the insertion site thoroughly, and maintain a sterile field throughout the procedure.
- Monitoring Infusion: Regularly monitor the IV site and infusion rate to ensure proper function and detect any signs of complications, such as infiltration, phlebitis, or air embolism. Adjust the flow rate as needed to maintain therapeutic goals.
- Discontinuing Infusion: Discontinue the IV infusion promptly once the treatment is completed or if any complications arise, such as signs of infection or allergic reaction. Remove the IV set carefully to avoid discomfort or injury to the patient.
- Documentation: Document all aspects of IV therapy, including the type of IV set used, insertion site, infusion rate, medications administered, and any adverse reactions or complications observed. Accurate documentation is essential for continuity of care and patient safety.
By following these best practices and guidelines, healthcare professionals can ensure safe and effective administration of IV therapy, promoting optimal patient outcomes and quality of care.